Background: In the 2017 version of the ELN recommendations (ELN2017), a comprehensive evaluation of karyotype and mutational status of specific genes (e.g. FLT3 and NPM1) allows to classify patients (pts) with Acute Myeloid Leukemia (AML) into 3 prognostically distinct risk groups (favorable, intermediate and adverse-risk). Before the publication of the ELN2017 guidelines, the Gruppo Italiano Malattie Ematologiche MAligne (GIMEMA) conducted a prospective trial (AML1310) in which prognostic classification relied on the risk assessment criteria (NCCN2009) at that time available. In this post-hoc analysis, we investigated the applicability of the ELN2017 risk stratification to the AML1310 study population.
Methods: After induction and consolidation, pts in complete remission (CR) were to receive autologous stem cell transplant (AuSCT) if categorized as favorable-risk (FR) (CBF-AML, NPM1-mutated) or allogeneic stem cell transplant (ASCT) if adverse-risk (AR) (FLT3-ITD, complex karyotype). Intermediate-risk pts (IR) were to receive AuSCT or ASCT based on the post-consolidation levels of MRD as measured by flow-cytometry. Baseline genetic/cytogenetic, together with RUNX1/RUNX1T1, CBFb/MYH11, NPM1, FLT3 mutational status (including the FLT3 allelic ratio for those positive) were used to retrospectively classify pts according to the ELN2017.
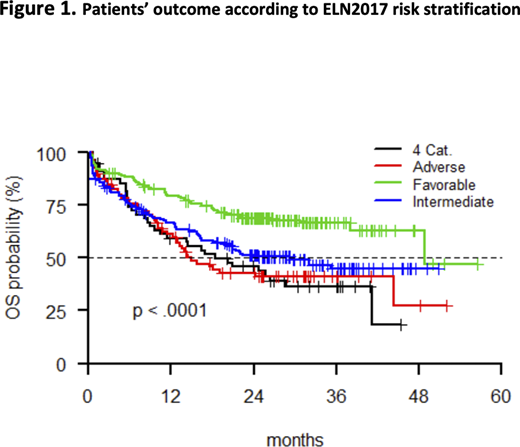
Results: All 500 pts, enrolled in the AML1310 trial, were included in the present analysis. Retrospective allocation was feasible in 445/500 (89%) cases and pts lacking crucial information for a proper ELN2017 assignment, defined a control group (ELN2017-NC). Median age was 49 (range 18-61). The re-assignmentaccording to the ELN2017, resulted in 186 pts (41.8%) belonging to the FR category (ELN2017-FR), 179 (40.2%) to the IR (ELN2017-IR) and 80 (18%) to the AR (ELN2017-AR) ones. Moreover, 55 (11%) pts were considered ELN2017-NC. Based on this process of re-assignment, 173 pts were reclassified according to ELN2017: 6 from NCCN FR (1 ELN2017-NC, 4 ELN2017-IR, 1 ELN2017-AR), 54 from NCCN IR (34 ELN2017-NC, 4 ELN2017-IR, 1 ELN2017-AR), and 113 from NCCN AR (20 ELN2017-NC, 38 ELN2017-FR, 55 ELN2017-AR) groups. After 1-2 cycles of induction, 361 (72%) pts obtained CR or CR incomplete (CRi): 163 (88.1%), 114 (65%), 45 (56.2%) and 39 (70%) in the ELN2017-FR, ELN2017-IR, ELN2017-AR and ELN2017-NC groups, respectively (p<0.001). Among 342 transplant candidates, 111/177 (82 [73.9%] ELN2017-FR, 19 [17.1%] ELN2017-IR, 2 [1.8%] ELN2017-AR, 8 [7.2%] ELN2017-NC) and 132/165 (25 [18.9%] ELN2017-FR, 61 [46.2%] ELN2017-IR, 25 [18.9%] ELN2017-AR, 21 [15.9%] ELN2017-NC) received AuSCT and ASCT, respectively (p<0.001). According to ELN2017 risk classification, the four groups significantly differed (p < 0.001) in terms of 2-years overall survival (OS) (68.8% vs. 51.3% vs. 45.8% vs. 42.8% for the ELN2017-FR, ELN2017-IR, ELN2017-NC, and ELN2017-AR groups, respectively). [Figure 1] Then, we investigated the impact of AuSCT and ASCT on each ELN2017 category; this evaluation was not possible for ELN2017-AR pts since only 2 of them received AuSCT. Among ELN2017-FR pts, a significant benefit of AuSCT over ASCT was observed (2-years OS of 83.3% vs. 66.7%, respectively; p=0.0421). In the ELN2017-IR group, AuSCT and ASCT performed equivalently (2-years OS of 73.9% vs. 70.8%, respectively). In univariate analyses, OS duration was shorter for pts from the ELN2017-AR (HR=2.203, CI 1.496-3.246; p<0.0001), ELN2017-IR (HR=1.796, CI 1.293-2-494; p=0.0005), and ELN2017-NC (HR=2.267, CI 1.488-3.228; p=0.0001). Multivariate model for OS prediction highlighted the role of age (HR=1.033, p<.0001), ELN2017 assignment and transplant (analyzed as a time-dependent covariate) (HR=0.674, p=0.0185), as the most significant prognostic variables.
Summary/Conclusion: In this GIMEMA AML1310 post-hoc analysis, we confirmed that the ELN2017 classification is able to accurately define pts that can benefit from different post-remission strategies. Specifically, AuSCT granted longer survival in FR pts, while for IR pts AuSCT and ASCT performed equally when minimal residual disease was used as a driver for opting between one of the two. In conclusion, ELN classification is a reliable grouping system that, combined with MRD assessment, helps addressing pts to the most appropriate treatment. Such an hypothesis will be prospectively challenged in the next GIMEMA trial AML1819.
Luppi:Abbvie: Consultancy; Novartis: Consultancy, Speakers Bureau; Gilead Sci: Consultancy, Speakers Bureau; Sanofi: Consultancy; Daiichi-Sankyo: Consultancy; MSD: Consultancy. Voso:Bristol Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Venditti:Pfizer: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company), Speakers Bureau; Amgen: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company); Jazz: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company); AbbVie: Consultancy, Honoraria, Other: TRAVEL, ACCOMODATIONS, EXPENSES (paid by any for-profit health care company); Janssen: Consultancy, Honoraria, Other: TRAVEL, ACCOMODATIONS, EXPENSES (paid by any for-profit health care company); Novartis: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company).
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal